Gambiaj.com – (BANJUL, The Gambia) – The National Health Insurance Authority (NHIA) has outlined its strategic priorities for 2026, placing emphasis on service expansion, sustainable financing, legal reforms, and improved access to healthcare services under The Gambia’s National Health Insurance Scheme (NHIS).
The NHIA aims to increase the number of insured individuals and achieve universal health coverage.
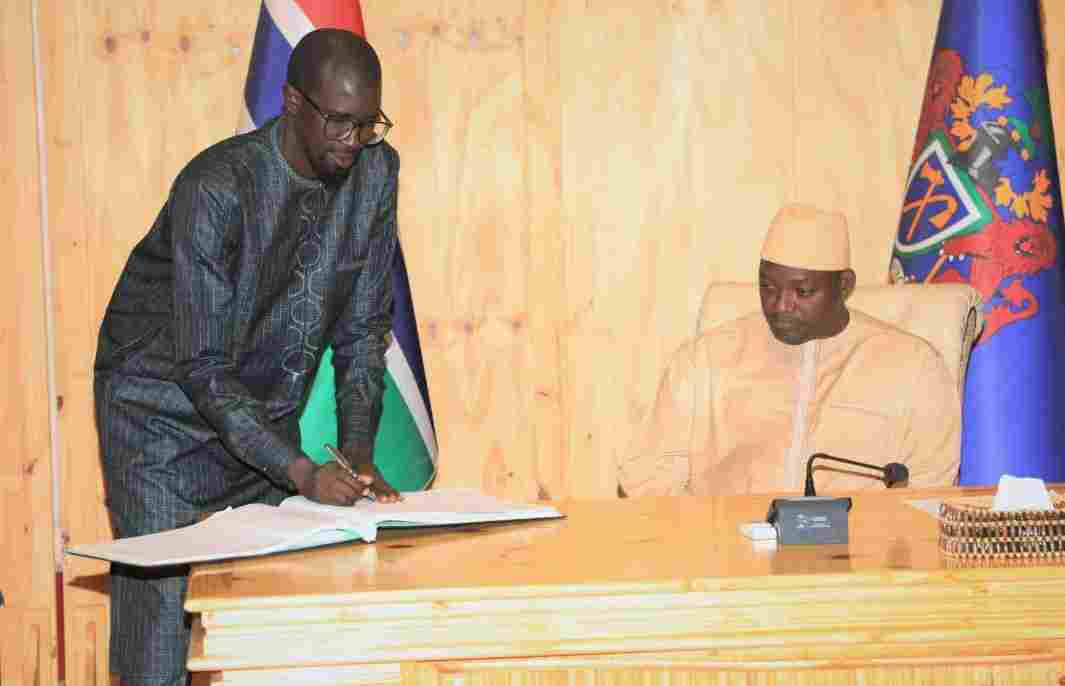
The priorities were presented during a Stakeholder Convergence held this week, where the NHIA took stock of progress made since the Scheme’s launch and engaged partners on plans for the year ahead.
Addressing stakeholders, the Chief Executive Officer of the NHIA, Bai Mass Saine, said the convergence provided an opportunity to reflect on lessons learned and to chart a clear path forward for building a strong, inclusive, and sustainable health insurance system.
“This Convergence provides an opportunity to present the National Health Insurance Authority’s strategic priorities for 2026,” the CEO said. “These priorities reflect where we are heading in the coming year and are based on our experience, the realities on the ground, and the reforms needed to build a strong and inclusive National Health Insurance Scheme for The Gambia.”
Expanding Coverage and Securing Sustainable Financing
According to CEO Bai Mass Saine, expanding services to reach more people—particularly those in rural and hard-to-reach communities—will be the Authority’s first priority in 2026. While acknowledging progress made so far, he said the focus would now be on ensuring essential health services are available across all regions.
“We have made significant progress, but the focus now is on reaching more people and ensuring essential health services are available in all regions,” he said, adding that continued support would be provided to contracted health facilities to improve access for women, newborns, and families.
Securing sustainable and predictable financing was identified as the second major priority. The CEO Saine stressed that the long-term success of the Scheme depends on reliable funding and said the Authority would work closely with government and development partners to strengthen financing mechanisms without compromising sustainability.
A third priority is the passage and implementation of amendments to the National Health Insurance Act. According to the CEO, the proposed amendments are intended to introduce mandatory contributions and reinforce the legal and financial foundations of the Scheme.
“Once passed, the Act will make the Scheme more equitable and capable of reaching every community in the country,” he said.
CEO Bai Mass Saine also highlighted administrative barriers that continue to limit access to the NHIS, particularly the linkage between NHIS registration and birth certificate issuance. He noted that this connection disproportionately affects non-Gambians, despite existing laws allowing everyone to register births.
“Currently, access to the NHIS card is limited by its connection to birth certification,” he said. “Addressing this will make the NHIS card more accessible to all eligible people, as intended by law.”
NHIS Growth, Tariffs, and Lessons Learned
The NHIA reported steady expansion of the Scheme since its launch. Services initially delivered through 13 contracted health facilities now cover more than 70 facilities nationwide, with service delivery extending to all regions of the country.
More than 50,000 women and newborns have received services under the Scheme so far, with claims paid on their behalf. The CEO said these figures translate into tangible improvements, including safer pregnancies, better maternal and newborn health outcomes, and reduced financial barriers to care.
“These figures represent real outcomes—safer pregnancies, improved maternal and newborn health, and reduced financial barriers to care for families,” he said.
Presenting details on the NHIS tariff structure, Director of Services Hasan Njie acknowledged persistent misunderstandings among stakeholders regarding what the Scheme covers. He said the Authority has published tariff summaries to enhance transparency and improve understanding.
“Even among key stakeholders who are supposed to know this very well, there seems to be a gap in understanding how the tariffs work,” Njie said.
He clarified that while certain medical services are reimbursed, medicines themselves are not currently covered under the Scheme. “We are not reimbursing for the medicines,” he said. “What we are paying for is the service and the specialized skills required to administer them.” He added that providers receive a 10 percent markup to help offset overhead costs.
Senior Quality Assurance and Benefits Manager Baba Njie also presented on the Scheme’s milestones, achievements, and lessons learned. He said the NHIS was established under the National Health Insurance Act passed in 2021, with institutional structures set up in 2022 and the benefits package developed in 2023.
According to him, more than half a million people have registered for NHIS cards since implementation began, following a pilot phase and subsequent nationwide rollout.
He noted that strong stakeholder engagement, a solid legal framework, digital claims processing, and continuous capacity building have been critical to progress, while challenges remain, including infrastructure gaps, data limitations, and delays in amending the NHIA Act.
“Health insurance is not just financing,” Baba Njie said. “It is protection, equity, and dignity.”
The convergence concluded with calls for continued collaboration among government institutions, health service providers, civil society organizations, and development partners as the National Health Insurance Scheme enters its next phase of implementation.